When her illness first began, Celeste Marx didn’t think much of it.
She felt more tired than usual and, at times, surprisingly weak. Then she started coughing — and whenever she coughed, she felt like she was going to throw up.
“I just thought, ‘Oh my gosh, what is happening to me?’” said Marx, who lives in south St. Louis County. “I just felt so incredibly lousy.”
Marx, 66, has lupus, a chronic autoimmune disease that makes it harder for her body to fight infection. When her temperature began to spike, she decided it was time to go to the hospital.
On a chilly evening in late March, her husband, Len, and their youngest daughter drove Marx to the emergency room at St. Luke’s Hospital In Chesterfield. At the time, only one visitor was allowed to wait in the ER, so Marx said goodbye to her family at the double doors. It was the last time she would see them for more than three weeks.
Not long after, Marx tested positive for the coronavirus — the first known case at St. Luke’s.
At home, Len Marx was trying not to panic, as he imagined his wife lying in a hospital bed, gasping for air. “Early on, I let my head get out in front of me,” he said. “I had to tell myself, ‘Stop, Len. Just take it one day at a time.’”
Staying connected
Tens of thousands of families across the U.S. have had loved ones hospitalized for COVID-19, and in most cases, they’ve been unable to see them. Many hospitals stopped allowing visitors to their intensive care units months ago to slow the spread of the virus. But the emotional toll of separation weighs heavily on those waiting at home, as they struggle to make medical decisions on behalf of their relatives.
Before the pandemic, family members would often sit at a patient’s bedside in the ICU, said Tracy Montauk, a registered nurse at St. Louis University Hospital.
“[They] could play music on their iPhone for their family members or tell them what was going on in the neighborhood or tell them a funny story about their dog,” said Montauk, who has worked in an ICU at SLU Hospital.
Sometimes, they would pin photos of their family member on the wall above their hospital bed — a person leaning over the railing of a cruise ship or posing in a flowered sundress.
Loading...
As these families watched doctors and nurses caring for their sick relatives, Montauk said, they also absorbed a lot of medical information and benefited from having “continuous and repeated conversations and questions answered in real time.”
But in late March, as hospitals prepared for a surge of COVID-19 patients in the St. Louis region, many health care providers suspended visitation. SSM Health, BJC Healthcare and Mercy began loosening visitor restrictions in June, but patients with COVID-19 still are not allowed to receive any visitors.
Hospital workers now speak with ICU families via video chat, dressed from head to toe in protective gear, including multiple face masks, a plastic face shield and a brightly colored medical gown.
“We would take the iPad into the room [and] give them a tour, like, ‘Here's the room they're in, here's the monitors, this is the medicine, these are the IV pumps,’” Montauk said.
These video chats are critically important for connecting with families, Montauk said. She recently co-authored an article with recommendations for ICU staff during the pandemic, such as acknowledging the difficulty of the situation and not being afraid to show emotion in front of families.
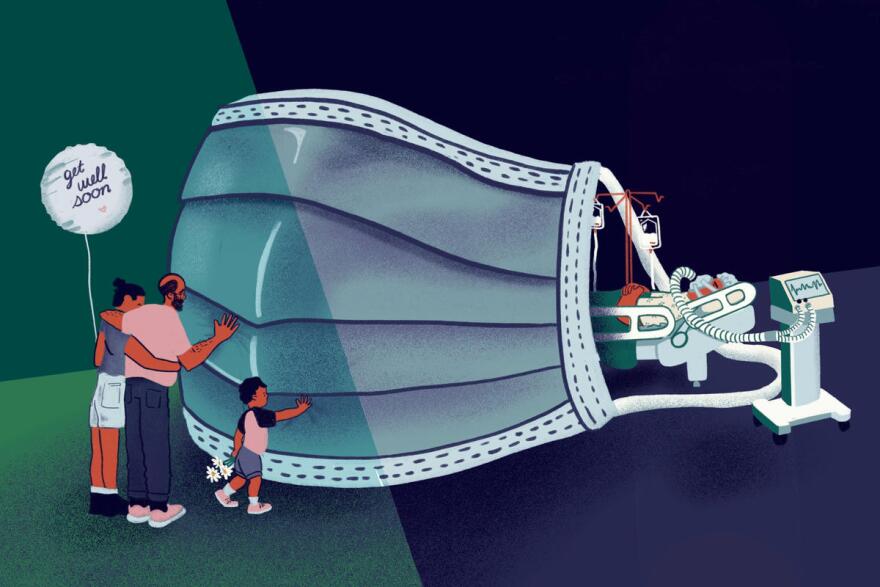
But despite the best efforts of medical workers, being isolated in the hospital with COVID-19 can be traumatic for patients and their families — especially when they’re near the end of life.
Jon Reynolds, an industrial mechanic who lives in St. Charles, faced this issue in March, after he and his wife, Deborah, 62, contracted the coronavirus.
“She has end-stage emphysema,” Reynolds said. “I knew if I called 911, they were going to take her, and I wouldn’t be able to be in the hospital with her. She’d be by herself and scared. So I did whatever I could to keep her home.”
But in the early hours of the morning, as Deborah Reynolds’ heartbeat grew more erratic and her oxygen levels dropped, her husband decided it was time to call an ambulance.
His wife has been admitted to the hospital a number of times in recent years for complications due to her emphysema, Reynolds said, and as her caretaker, he prefers to stay close by.
“This is my wife's life,” he said. “Now, I can't be there. I can't hold her hand. I can't witness what's going on. I just have to take a stranger's word for it.”

Deborah Reynolds was discharged after about two weeks at St. Joseph’s Hospital, but she hasn’t fully recovered.
“I nursed her back, but it really did some damage to her lungs,” Reynolds said. “She's not the same person anymore. She lost a lot of memory and she just, she's not there.”
Clinical social worker and therapist Velma Bell works with trauma patients and their families in south St. Louis. Caregivers may struggle with feelings of helplessness, she said, especially when they’re not able to oversee the care of their sick loved ones.
Being present when a loved one is ill is also an important part of our rituals around sickness and death, Bell added, and for some, it provides a sense of purpose.
“I think we believe a voice or a touch or a smell can somehow provide relief and support for that person to fight and hold on,” Bell said. “We want to believe that we can somehow change outcomes, and sometimes we're just not able to do that.”
'Is Mom going to die today?'
As Celeste Marx’s condition slowly deteriorated at St. Luke’s Hospital in Chesterfield, Len Marx waited at home, trying to gather as much information as possible.
He started calling the hospital three or four times a day — and whenever he talked to the doctors and nurses, he frantically scribbled down as much as he could in a spiral notebook.
“I was writing like a high school student, ‘OK, tell me more. Tell me more,’” Marx said. “The learning curve on all this — I never knew what an oxygen saturation level was until this.”
Marx worried that he might miss a call from the hospital, so he started sleeping with his cellphone on his pillow.

Then, a week after Celeste Marx was admitted, her doctor called. She wasn’t getting enough oxygen and needed to be put on a ventilator as soon as possible. Before being intubated, however, she had asked to see their priest.
After Marx hung up the phone, his youngest daughter, Lisa, who has autism, turned to him with a question.
“We got the call that [Celeste] was going to the ICU and Lisa, with a serious kind of voice, said, ‘Is Mom going to die today?’” Marx said. “Boy, does that hit you.”
While Celeste Marx was being put on a ventilator, 30 miles away in East St. Louis, Amanda Blackwell was struggling to breathe.
Blackwell works in admissions in the St. Alexius Hospital emergency department in St. Louis — and in late March, the 38-year-old started feeling ill.

At first, she thought it was just a bad head cold. Her doctor wrote her a prescription for antibiotics and told her to rest at home.
But Blackwell kept feeling worse. At one point, she remembers crawling to the bathroom, gasping for air.
“My mother was calling me every day, all day,” Blackwell said. “I remember talking to her, and she was crying. She said, ‘Call them right now or I'm calling.’ She begged me, and I finally called 911.”
Blackwell tested positive for the coronavirus at St. Elizabeth’s Hospital in O’Fallon, Illinois, and the next day, she was put on a ventilator. She woke up 23 days later.
“I was just terribly, terribly scared,” Blackwell said. “I was really confused. One of the nurses was really sweet, and she brought her phone in there to let my mom talk to me. When she FaceTimed me, I kept looking at the lady shaking my head, like I don't know who this is. It was my mother. I had no idea who she was.”
The ventilator had strained her vocal cords, and Blackwell wasn’t able to speak for days after waking up. She remembers a nurse sitting by her bedside, holding up a hand and asking, ‘Do you know what this is?’"
Blackwell spent about a month in the rehabilitation unit at St. Joseph’s Hospital in Highland, Illinois, learning how to walk and talk again. When she was finally discharged in late May, her mom was waiting to surprise her.
“Oh my god, I just cried,” Blackwell said. “I just grabbed her, didn't want to let her go.”
Her mother had waited at home for weeks, knowing that she might never see her daughter again — and it took on a serious toll on her, Blackwell said. Even now, she won’t discuss the experience with anyone but her daughter.
“Not too long ago, I had that moment where I kind of broke down and I asked my mom, 'Why did this happen to me?’” Blackwell said. “And she said, ‘Why not? God gave you a second chance.’ That stuck with me. A lot of people didn't make it, but I’m alive.”

In early April, Celeste Marx was the first COVID-19 patient who had been on a ventilator to be discharged from St. Luke’s Hospital.
She tried not to cry as a nurse wheeled her through a hallway lined with applauding hospital workers — to the sliding glass doors where her husband was waiting for her.
“I was even afraid to touch him, but he just came right over to me and kissed me,” Marx remembers. “That was so wonderful, just true joy.”
Months later, Marx feels guilty knowing what her family went through while she was hospitalized, and she believes those weeks were harder for them than for her.
“Unfortunately, COVID is still with us,” she said. “It’s hard on the patient, and it’s so hard on the family, because you are isolated. You’re isolated.”
Follow Shahla on Twitter: @shahlafarzan
Send questions and comments about this story to feedback@stlpublicradio.org





